Managing Hot Flashes Naturally in Perimenopause: Hormone and Non-Hormone Options Explained
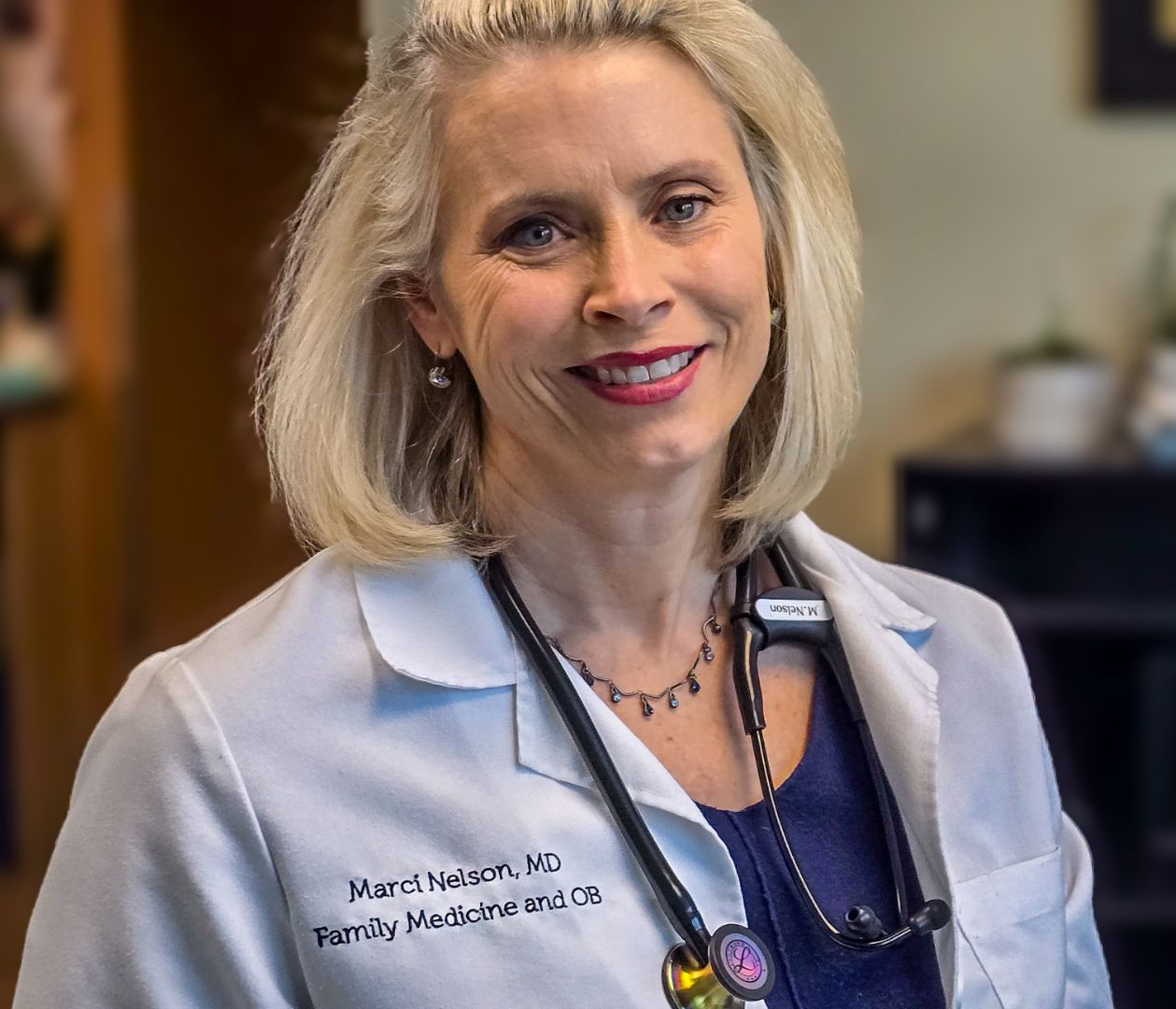
- Dr. Marci Nelson, MD, MSCP
- Dec 6, 2025
- 5 min read
Hot flashes and night sweats, known medically as vasomotor symptoms (VMS), are among the most common and disruptive symptoms of perimenopause. For many women, they begin years before the last menstrual period and can interfere with sleep, focus, and daily comfort.
While hormone therapy (HT) remains the most effective treatment, it is not right for everyone. Some women prefer managing hot flashes naturally with non-hormonal options, while others have health conditions that make hormone use less suitable. Fortunately, current research offers a variety of evidence-based choices for relief.
“Hormone therapy was once routinely used to treat menopause symptoms and protect long-term health. Then large clinical trials showed health risks. What does this mean for you?” - Mayo Clinic
This article summarizes both hormone and non-hormone therapies for vasomotor symptoms, based on findings from the Cleveland Clinic Journal of Medicine and guidance from The Menopause Society, ACOG, and other respected medical sources.
Understanding Hot Flash Symptoms in Perimenopause
Hot flashes and night sweats occur when changing estrogen levels affect the hypothalamus, the part of the brain that regulates temperature. As estrogen fluctuates, the body’s temperature “set point” narrows, making small increases in body heat trigger sweating, flushing, and sudden warmth.
According to The Menopause Society, up to 75% of women experience hot flashes during the menopausal transition, and about one in three describe them as moderate to severe in intensity.
For some, these episodes are brief and manageable. For others, they cause chronic sleep disruption, fatigue, and anxiety. Recognizing how common and treatable these symptoms are is an important first step toward relief.

Hormone Therapy: The Most Effective Option for Many Women
Estrogen therapy is considered the gold standard for treating vasomotor symptoms. Estrogen therapy has been shown to reduce hot-flush frequency by approximately 70 %–80 % in clinical trials.
For women under 60 or within 10 years of menopause onset, and without contraindications, the benefits generally outweigh the risks.
When Hormone Therapy May Help
Frequent or severe hot flashes or night sweats disrupting sleep or work
Early or premature menopause (before age 45)
Coexisting symptoms such as vaginal dryness, low libido, or mood changes
Good cardiovascular and breast health
When Hormone Therapy May Not Be Recommended
Women with a history of breast or uterine cancer, heart attack, stroke, blood clots, or liver disease should usually avoid hormone therapy. In these cases, non-hormonal options are preferred.
For many women, the choice depends on individual risk factors, comfort level, and how much symptoms affect quality of life.
Managing Hot Flashes Naturally with Evidence-Based Non-Hormone Therapies
Recent research, including a 2024 review in the Cleveland Clinic Journal of Medicine, highlights several non-hormonal treatments that can meaningfully reduce hot flashes and night sweats.
1. Cognitive Behavioral Therapy (CBT)
CBT is a structured form of therapy that helps women change how they perceive and respond to hot flashes.
It does not stop the physical occurrence of hot flashes but reduces their emotional and sleep impact.
The North American Menopause Society (2015) recommends CBT as an effective non-hormonal treatment option for hot flushes and night sweats. Online or group-based CBT programs can also be effective. CBT reduced subjective frequency of night sweats by an average of 39 % and reduced objectively measured hot flushes… in some trials.
2. SSRIs and SNRIs
Certain antidepressants, used at lower doses than for depression, can meaningfully reduce hot-flash frequency. Evidence supports:
Paroxetine 7.5 mg nightly — the only FDA-approved nonhormonal drug specifically for vasomotor symptoms; dose and indication per the official label. FDA Access Data
Venlafaxine 37.5–75 mg daily — randomized trials show reductions in hot-flash frequency and interference; networked evidence places it among the most effective nonhormonal options. JAMA Network+1
Escitalopram 10–20 mg daily — an RCT in JAMA found significantly greater odds of ≥50% reduction in hot-flash frequency versus placebo. JAMA Network
Desvenlafaxine 50–100 mg daily — trials report clinically meaningful reductions in frequency and severity of hot flashes by 55 to 69%. PMC
3. Gabapentin and Pregabalin
Gabapentin and pregabalin, originally developed to treat nerve pain and seizures, have been shown in clinical trials to reduce hot-flash frequency by about 45% to 60%.
In one JAMA Internal Medicine trial, gabapentin 900 mg per day decreased hot flashes by nearly half compared with placebo. Lower doses, such as 300 mg at bedtime, are often used in clinical practice and may also help women who struggle with sleep disruption from night sweats.
Common side effects include drowsiness and mild dizziness, which can improve as the body adjusts to treatment (Cleveland Clinic Journal of Medicine, 2024; JAMA Internal Medicine, 2006).
4. Clonidine
Clonidine, a blood pressure medication, has modest benefit in reducing hot-flash frequency but is less effective than newer options.
Due to side effects such as dry mouth, fatigue, and low blood pressure, it is often used only when other therapies are unsuitable.
5. Fezolinetant or Elinzanetant
Fezolinetant and Elinzanetant are both neurokinin-3 (NK3) receptor antagonists that target the brain’s thermoregulation center. These are non-hormonal. Fezolinetant was approved by the FDA in May 2023 and Elinzanetant was approved by the FDA in October 2025, both for the treatment of moderate to severe vasomotor symptoms (hot flashes and night sweats) associated with menopause.Source: Fezolinetant FDA approval announcement, dosing and safety details are in the press release.
FDA: https://www.fda.gov/news-events/press-announcements/fda-approves-novel-drug-treat-moderate-severe-hot-flashes-caused-menopause
How well these work: Phase 3 SKYLIGHT trials demonstrated significant reductions in hot-flash frequency and severity compared with placebo, with improvements evident by week 4 and maintained through week 12. A 2024 clinical review summarizes that fezolinetant 45 mg produces meaningful symptom reductions and notes a rapid onset of benefit.
CCJM clinical review (nonhormone therapies overview): https://www.ccjm.org/content/91/4/237
SKYLIGHT efficacy publication (PubMed record): https://pubmed.ncbi.nlm.nih.gov/36924778/
Lancet abstract (SKYLIGHT trial): https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)00085-5/abstract
Lifestyle and Behavioral Approaches
Non-pharmacologic strategies remain an essential foundation for managing symptoms. While they may not eliminate hot flashes completely, they support better sleep, mood, and overall well-being.
Practical steps include:
Keeping indoor temperatures cool and wearing light, breathable clothing
Reducing alcohol, caffeine, and spicy foods that can trigger hot flashes
Maintaining a healthy body weight
Practicing paced breathing (slow, steady breathing for several minutes during an episode)
Engaging in regular aerobic and strength exercise
Trying mind-body practices such as yoga, meditation, or tai chi to help regulate stress hormones
These approaches are low-risk and can complement any medical treatment plan.
Comparing Hormone and Non-Hormone Therapies
Treatment Type | Typical Symptom Reduction | Time to Notice Improvement | Key Considerations |
Estrogen Therapy | 70–90% | 1–4 weeks | Most effective; not suitable for all women |
SSRIs/SNRIs | 50–60% | 2–4 weeks | May also improve mood and sleep |
Gabapentin | 45–60% | 1–2 weeks | Helpful for nighttime symptoms |
Fezolinetant/ Elinzanetant | 50–60% | 1–2 weeks | Non-hormonal; monitor liver function |
CBT | 40–50% (perceived reduction) | Gradual | Improves coping and sleep quality |
Lifestyle Changes | Variable | Ongoing | Foundational for all approaches |
Working With Your Clinician
Selecting the right treatment starts with an honest conversation about your medical history, risk factors, and personal preferences.
Many women benefit from combining approaches: lifestyle adjustments, mind-body strategies, and either hormonal or non-hormonal medications when symptoms remain disruptive.
In my own work with women in perimenopause, I see that clarity and education often reduce anxiety around treatment decisions. Knowing that safe, effective options exist, both hormonal and non-hormonal, can bring a sense of calm and control back into your daily life.
You do not need to “tough it out.” Relief is possible, and finding what works best for you is a process worth taking step by step.
References
Avis NE, et al. Nonhormone therapies for vasomotor symptom management. Cleveland Clinic Journal of Medicine. 2024;91(4):237–245. https://www.ccjm.org/content/91/4/237
The Menopause Society. Nonhormonal Management of Menopausal Symptoms: Position Statement. https://www.menopause.org/
American College of Obstetricians and Gynecologists. Hormone Therapy for Menopause. https://www.acog.org/womens-health/faqs/hormone-therapy-for-menopause
Mayo Clinic. Menopause treatment: Hormone and nonhormone options. https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
.png)

Comments