Sleep and Perimenopause: Why It Changes and What Can Help You Rest Again
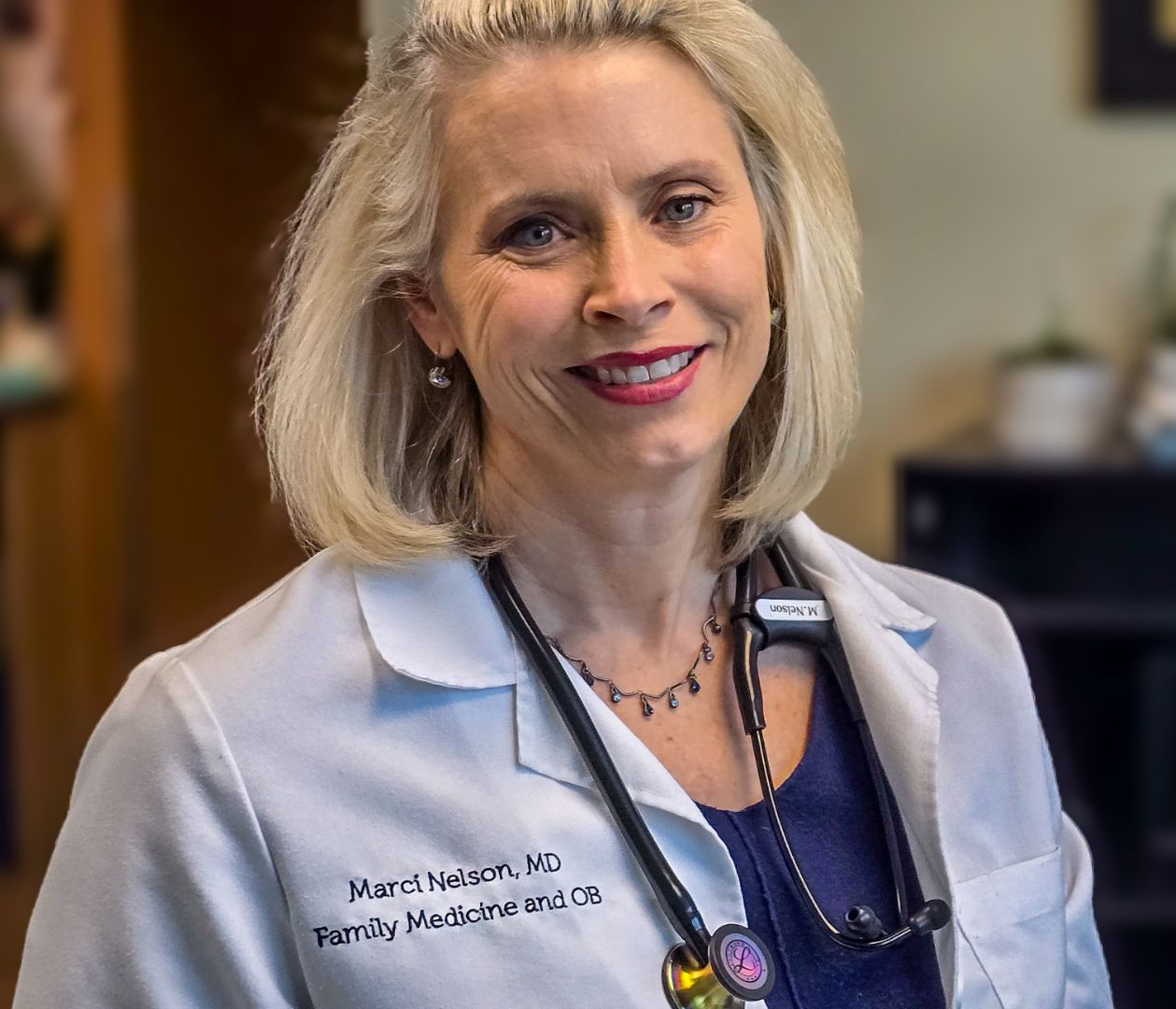
- Dr. Marci Nelson, MD, MSCP
- Nov 9, 2025
- 4 min read

If you find yourself wide awake at three in the morning, wondering why your body suddenly feels alert when it should be resting, you are not alone. Many women in their forties and fifties tell me the same story. Their sleep that once came easily now feels unpredictable.
Sleep changes are one of the most common concerns during perimenopause. Hormone shifts, stress, and the pace of daily life can all affect the body’s ability to rest deeply. The good news is that these changes are understandable, and there are ways to improve them. Once you learn what is happening in your body, sleep becomes something you can work with rather than struggle against.
Why Sleep Changes During Perimenopause
Perimenopause is a natural transition that usually begins several years before the final menstrual period. During this time, estrogen and progesterone levels fluctuate rather than declining smoothly. Both hormones have important effects on how the brain and body manage rest.
Estrogen helps regulate body temperature and serotonin. When levels shift, body heat rises and night sweats or hot flashes can interrupt deep sleep.
Progesterone has a gentle calming influence on the brain. As it decreases, falling asleep or staying asleep can take more effort.
Melatonin, the hormone that signals bedtime, also tends to decline with age. Changing cycles can alter its timing, leading to lighter or shorter sleep.
Studies from the North American Menopause Society report that between forty and sixty percent of women in perimenopause notice new sleep difficulties. For some, the issue is falling asleep. For others, it is waking up in the middle of the night and being unable to return to rest.
Common Sleep Disruptors

Night sweats and temperature spikes
Sudden waves of heat can jolt you awake multiple times a night. Even small temperature changes can be disruptive. Lowering the thermostat, using light bedding, and wearing breathable sleepwear can make a real difference.
Anxiety and mood changes
Fluctuating hormones can influence neurotransmitters such as serotonin and GABA, which affect calmness and mood. You may feel unsettled at bedtime even when nothing is outwardly wrong. Gentle relaxation or mindfulness before bed can help your nervous system shift gears.
Sleep fragmentation
Some women fall asleep easily but wake during the early morning hours. The body’s temperature rhythm, caffeine intake, or stress hormones can all contribute. Keeping a consistent bedtime and wake time can help reset this rhythm.
Life load
Midlife often comes with heavier responsibilities: caring for aging parents, supporting teenagers, managing work transitions. These pressures layer on top of hormonal changes and make true rest feel out of reach. Recognizing this stage of life as demanding, and being kind to yourself, is part of the solution.
When several of these factors overlap, the body becomes stuck in a pattern of light, restless sleep. Fatigue then affects mood, focus, and even appetite, creating a cycle that feels hard to break.
Evidence-Based Strategies to Support Better Sleep
Improving sleep during perimenopause often requires several small steps that work together. Each woman’s pattern is unique, so what helps one person may not help another. Start with gentle adjustments and build from there.
Create a calm, cool environment
Aim to keep your bedroom between sixty and sixty-seven degrees. Turn off bright lights, reduce noise, and avoid screens right before bed. Alcohol and large meals can raise body temperature, so give yourself at least two hours between eating and lying down.
Build a consistent bedtime ritual
Your brain learns by repetition. Choose a few quiet activities that signal rest—reading, light stretching, journaling, or slow breathing. Begin them at the same time each evening. Consistency helps your body recognize when it is safe to let go of the day.
Manage stress hormones
Mind-body practices such as yoga, meditation, or paced breathing have been shown to lower cortisol, the stress hormone that can interfere with sleep. Even five minutes of slow, intentional breathing can calm the heart rate and quiet the mind.
Understand your hormonal rhythm
If sleep problems coincide with hot flashes, mood changes, or cycle irregularity, it may be helpful to talk with your clinician. Some women benefit from hormonal therapy, while others find relief through cognitive behavioral therapy or targeted lifestyle adjustments.
Review medications and supplements
Over-the-counter sleep aids and herbal supplements are widely advertised, but they are not all effective or safe for everyone. Some may interact with prescription medications or carry side effects. Always discuss new products with a licensed healthcare provider before adding them to your routine.
When to Seek Additional Support
If you are lying awake more than three nights a week despite making healthy changes, it may be time to seek guidance. Persistent insomnia, unmanageable hot flashes, or heavy reliance on sleep aids are signs that more help could be useful.
In coaching sessions, we make sure to discuss your sleep patterns; bedtime routines, caffeine use, and how symptoms like temperature changes or awakenings affect rest. Together we build a plan that fits your body’s rhythm and daily life.
Coaching is not a replacement for medical care, but a companion to it. The goal is to understand your unique triggers and build a plan that restores both confidence and rest.
How Perimenopause Coaching Can Help You Sleep Better
As a physician and Menopause Society Certified Practitioner, my approach blends clinical knowledge with empathy. Together, we:
Identify the underlying causes of disrupted sleep.
Review proven strategies, from sleep hygiene to nutritional and hormonal options.
Build habits that are realistic for your daily life.
Reassess progress over time and make adjustments that keep you improving.
Many women tell me that once they understand why their sleep changed, their frustration eases. Knowledge brings calm, and calm supports rest.
If you would like to learn more about how personalized menopause coaching can complement your care, visit the Perimenopause Coaching Program page.
Taking the First Step Toward Better Sleep
Sleep is not a luxury; it is one of the foundations of health. When it falters, everything feels harder. You deserve nights that restore you and mornings that feel clear again.
If you have been told to simply wait it out, know that you have options. There are effective, evidence-based ways to improve sleep during perimenopause, and you do not have to navigate them alone.
Ready to start sleeping better? Book your free 10-minute discovery call to explore what might work for you.
.png)

Comments